
Parent to Parent: Real life with a child with blood cancer
Edmonton AB
Canada
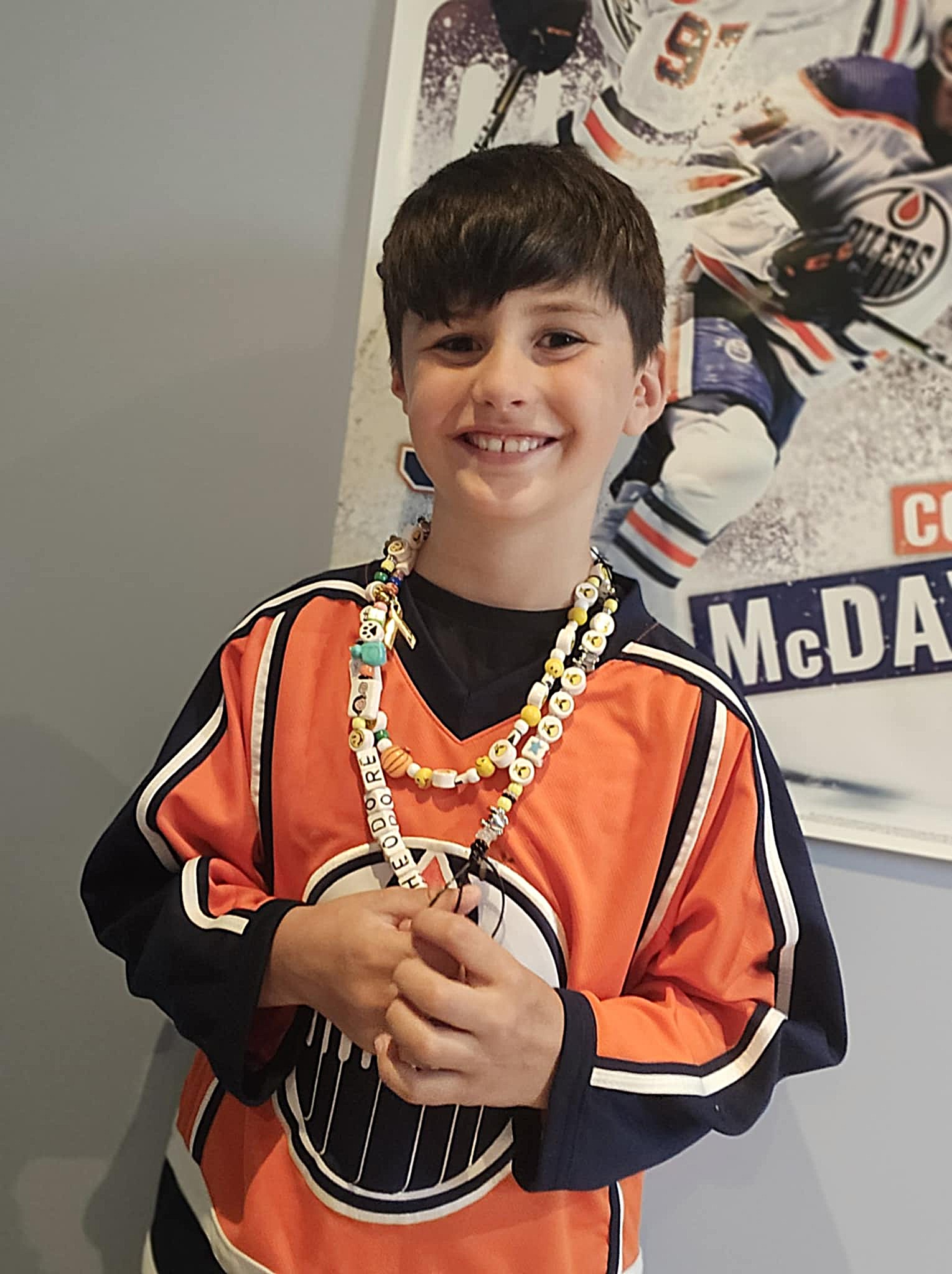
Rechelle and Shane Ramsay on parenting Theo, 5, with lymphoma
This is Rechelle and Shane Ramsay’s story of their family’s experience when their son, Theo, was diagnosed with lymphoma at age 5. It is the first in a new series we call, “Parent to Parent: Real life with a young child with blood cancer.”


Seeking trauma relief
“His schedule was suddenly out the window. He was thinking ‘what is the new routine? What are these machines? Why am I getting poked with needles so much? Where is my comfy family stuff, the food I grew up eating?” Rechelle recalls.
“During chemotherapy, Theo became a very different kid. He was angry all the time, you couldn’t regulate him. He would cry hours straight, sometimes he would kick, punch or try to bite me,” says Rechelle, adding that sometimes she would also cry during it. “It was OK, he was seeing that Mom’s hurt and sad, too, he’s not the only one.”
Still, nothing helped. “He wouldn’t talk. A therapist saw him at the hospital, and he just cried.” A doctor suggested a temporary anti-anxiety medication to get through the worst of it; Rechelle resisted that for weeks, something she says she regrets.
As the struggle intensified, Rechelle decided to let Theo try the meds. “I didn’t want the trauma of cancer to be worse for him than it had to be,” she said. His anxiety dropped, he was able to talk and connect again. “I wish I’d done it sooner. I was stubborn, I thought ‘we can figure this out.’”

Holding down the home front
Rechelle and Shane had a lot to figure out, all at once. A welder who unfortunately wasn’t able to take much time off, Shane needed to care for their younger son Oliver, 3, who was acting out at home. “Potty training went out the window. Ollie was throwing toys; he couldn’t understand where Theo went.”
Grandpa (Shane’s dad) moved in to help care for Ollie and the family dogs, bringing much needed practical support. Still, they grappled with the complexities of navigating a three-generation household with a giant hole – mom and son away every second week for four months, including over the Christmas holiday.
“It was hard for Shane to put on a facade as strong breadwinner when he wasn’t able to be with his sick kid at the hospital,” says Rechelle. The couple made a point of speaking honestly and privately every day throughout the experience about what their respective days were like and how they were feeling. “Sadly, I met parents in the cancer ward who got divorced while their kid was getting chemo,” she remembers.
Navigating other people’s reactions

“Shane is good at asking ‘what do we need as a family?’ When I felt drained having to tell everyone details about our cancer journey all the time, he said ‘you don’t have to.’ He and I decided what we’d communicate to who and when.” Shane updated immediate family and close friends via a group text, and Shane’s dad updated his relatives.
“Navigating other people’s reactions is the hardest part of breaking the cancer news,” Rechelle recalls, “while trying to keep yourself composed. While some people were very emotional , jumping to negative thoughts, other family members were like ‘do you need meals? Can we watch Ollie, can we pack for you?”
The night before each biweekly trip to the hospital, the home of Rechelle’s sister was a safe haven, a planned sleepover where she could “unload all my feelings while the cousins were playing…You have to be able to vent without burdening your kids or spouse.”
‘Family life’ in hospital
Rechelle had a bed in Theo’s hospital room. (“We played long sleepover.”) “My goal every morning was to get to the end of that day with as much planned as possible,” says Rechelle. “So after chemo and lunch, when Theo was alert for an hour or two, I’d have something planned for that day, some activity,” says Rechelle.
She dressed up Theo’s IV pole like a Christmas tree, played skateboarding and pirate ship moving him around the ward. Every evening after dinner she and Theo would Facetime with Shane, Grandpa, Ollie and the dogs.

Rechelle tried to keep family rules the same in hospital as at home, too. “’OK, your life is going crazy but you’re still not allowed unlimited video gaming or ice cream every day.” She admits “it’s hard to get your head around at first, but it is ok to say ‘no’ to a child with cancer… Kids need to feel a sense of control, too, and boundaries and routines help with that.”
Rechelle and Theo made friends in the pediatric cancer ward (“I was close with some parents, and the teenagers would play Minecraft with Theo”) but she admits there was tension at times. “Theo responded very well to his treatment; other kids and babies did not.” She stays in touch with some of those parents still today.
_________________________________________________________________________________
Been there, done that: Insider tips
- Take mental health breaks every day. Even in the hospital. Just because you’re the parent doesn’t mean you’re the only one who can entertain, soothe, or watch your sick child. Accept the offers of nurses and family to relieve you while you go for a coffee, a short walk, or a rest. (“It helped to step outside and see normal humans living normal lives,” says Rechelle.)
- Explore all treatment options – and not just for the cancer. Be open minded to anything that lessens the emotional toll it can take on your child, siblings, spouse and yourself. Minimize where you can the trauma that cancer creates.
- Advocate medically, with empathy – Don’t be afraid to ask to see a different doctor or get a different test or treatment plan – but also remember that “healthcare professionals are trying their best; they’re frustrated, too” says Rechelle.
- You don’t owe anyone constant updates – Put up healthy boundaries when people outside your inner circle are asking for details on the cancer. Ask immediate family to help share the load of communication.
- Control what you can. “Initially I felt defeated, that there was nothing I can do… once you accept you cannot control everything, that is the first step to moving forward,” says Rechelle. Then control what you can: a predictable routine, family rules, scheduled calls, etc.
- Take the pressure off – Pick your battles; you cannot do it all as a parent. (For example, “I told my husband it’s fine to make mac and cheese for days in a row while we’re going through all this,” says Rechelle.)
- Keep a journal(s) for you and/or your child to express all kinds of feelings, as well as mark milestones during the cancer journey, new friends, activities, maybe “you can journal what went wrong today and how I wish it went differently,” Rechelle suggests.
- Schedule emotional support. While it’s great to ask for and receive practical support (dog walking, babysitting, groceries, etc.), do not neglect emotional support! Set regular phone or in-person dates with someone you know will listen with compassion. If you don’t have that, reach out to an organization like The Leukemia & Lymphoma Society of Canada for personalized support including a one-on-one phone match with another parent whose child has gone through blood cancer.
